Bone Densitometry at Delhi Disc & Rheumatology Clinic: A Game Changer in Bone Health Assessment
Let’s get straight to the bone of the matter — Bone Densitometry at Delhi Disc & Rheumatology Clinic is not just a fancy-sounding procedure. It’s a powerful, precise and downright essential tool in the world of modern medicine. If you’ve been wondering why your doctor keeps talking about T-scores and DEXA scans like they’re the next best thing since sliced bread, buckle up. We’re diving deep into what bone densitometry is, why it matters and why Delhi Disc & Rheumatology Clinic might just be the best place to get it done.
What Exactly Is Bone Densitometry?
Before we spring ahead, let’s warm up with the basics. Bone densitometry, also known as a DEXA or DXA scan (short for Dual-Energy X-ray Absorptiometry — try saying that three times fast), is a non-invasive test that measures bone mineral density (BMD). Simply put: it tells us how strong your bones are.
Think of it like a bone report card. It helps doctors detect osteoporosis, evaluate fracture risks and decide if treatment is needed. And guess what? It does all this in under 30 minutes, without breaking a sweat.
Why Bone Densitometry at Delhi Disc & Rheumatology Clinic Is Different
Sure, you could get a bone scan at a big hospital, but here’s the deal — Delhi Disc & Rheumatology Clinic brings something extra to the table:
- State-of-the-art DEXA technology – fast, accurate and low-radiation.
- Experts in rheumatology and orthopedics – they know bones like bakers know bread.
- Personalized care plans – because no two skeletons are exactly the same.
- Central location in Delhi – super convenient whether you’re in Noida, Gurgaon or South Delhi.
And let’s not forget the vibe. This clinic isn’t cold or impersonal — it’s warm, professional and genuinely focused on patient wellbeing.
Who Needs a Bone Densitometry Test?
Great question! Bone density scanning isn’t just for the elderly. In fact, if you check even one of the boxes below, you might want to consider it:
- Women over 50 or post-menopause
- Men over 70
- Anyone with a family history of osteoporosis
- People who have broken bones easily in the past
- Long-term steroid users
- Individuals with rheumatoid arthritis or other autoimmune conditions
- Folks with low body weight or eating disorders
- Smokers and heavy drinkers
Yes, bone health can go downhill quietly, but a bone densitometry at Delhi Disc & Rheumatology Clinic will catch it before it’s too late.
The Science Behind the Scan
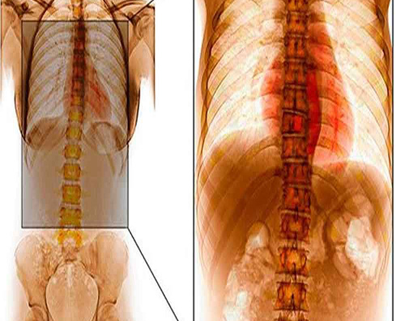
Now, for the nerds (we see you and we respect you), here’s how bone densitometry actually works:
- The scanner emits two X-ray beams at different energy levels.
- One beam gets absorbed by soft tissue; the other by bone.
- By subtracting one from the other, the machine calculates your bone density.
It’s like bone mathematics — but way cooler and done in seconds.
Interpreting the Results: What Do T-Scores Mean?
You’ve had the scan. Now what?
Here’s what your results might say:
| T-Score | What It Means |
| Above -1 | Normal bone density |
| -1 to -2.5 | Low bone mass (osteopenia) |
| Below -2.5 | Osteoporosis (time for action!) |
Your doctor will also consider Z-scores if you’re younger than 50, which compare your BMD to what’s expected for your age, sex and size.
Think of it this way: if T-scores are your final exam results, Z-scores are the class average comparison.
What Happens If Your Results Aren’t Great?
If your scan shows signs of low bone density or osteoporosis, the team at Delhi Disc & Rheumatology Clinic won’t just hand you a pamphlet and send you packing. You’ll get a tailored treatment plan which might include:
- Calcium and vitamin D supplements
- Weight-bearing exercises
- Lifestyle modifications (yes, quitting smoking helps!)
- Prescription medications like bisphosphonates
- Follow-up scans to track progress
And here’s the kicker: early detection can literally prevent fractures and permanent disability. That’s no small deal.
Bone Densitometry for Seniors: Essential, Not Optional
Let’s be real — as we age, our bones get a little tired. Seniors are especially vulnerable to silent bone loss. A simple fall could lead to a hip fracture, hospital stay or worse.
That’s why bone densitometry at Delhi Disc & Rheumatology Clinic is often recommended as a routine part of aging well. It’s preventive medicine at its best.
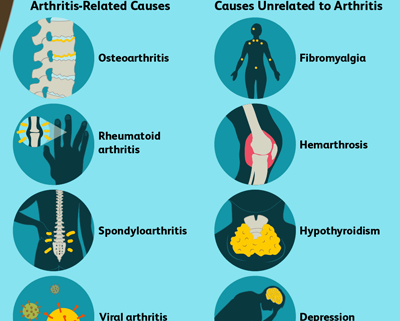
Bone Density and Rheumatologic Disorders
Did you know that conditions like rheumatoid arthritis, lupus and ankylosing spondylitis can mess with your bones?
Chronic inflammation wears away at bone over time, and the meds used to control these diseases can also weaken bone density.
At Delhi Disc & Rheumatology Clinic, the experts know this inside and out. They’re trained to balance disease management and bone health — that’s the double win you want.
How to Keep Your Bones Happy and Dense
While we’re on the topic, here are some bone-boosting hacks you can start today:
- Eat foods rich in calcium (hello, paneer and almonds!)
- Get your daily dose of sunshine for Vitamin D
- Lift some weights or do resistance training
- Avoid excessive alcohol and caffeine
- Stay active — bones love movement!
But remember: even if you feel fine, bone loss can happen silently. That’s why routine bone densitometry at Delhi Disc & Rheumatology Clinic is a smart move.
Why Choose Delhi Disc & Rheumatology Clinic for Bone Densitometry?
Let’s break it down:
- ✅ Accuracy – top-tier DEXA machines leave no bone unscanned
- ✅ Expertise – real rheumatologists, not random technicians
- ✅ Speed – in and out in under an hour
- ✅ Comfort – kind, professional staff and a no-pressure environment
- ✅ Trust – thousands of patients served across Delhi-NCR
Honestly? They’re not just scanning bones. They’re safeguarding futures.
Conclusion: Strong Bones, Strong Life
Bone health might not be the sexiest topic at a dinner party, but it’s crucial. With Bone Densitometry at Delhi Disc & Rheumatology Clinic, you’re not just getting a scan — you’re getting answers, early intervention and peace of mind.
Whether you’re dealing with symptoms, at high risk or just want to play it safe, don’t wait until the cracks show. Schedule a scan. Know your score. Own your health.
Frequently Asked Questions
1. Is bone densitometry painful?
Nope! It’s a completely painless, non-invasive procedure. You lie on a table, stay still for a few minutes and you’re done.
2. How long does a bone density scan take at Delhi Disc & Rheumatology Clinic?
Typically around 20–30 minutes from check-in to results. Super efficient!
3. How often should I get a bone densitometry scan?
If you’re at risk, every 1–2 years. Your doctor will guide you based on your condition and treatment progress.
4. Is it safe to do bone densitometry regularly?
Yes. The radiation is minimal — far less than a chest X-ray or a cross-country flight.
5. What’s the cost of a bone densitometry at Delhi Disc & Rheumatology Clinic?
Costs vary slightly depending on insurance, but they’re known for being affordable and transparent.
6. Can men get osteoporosis too?
Absolutely. It’s less common but still very real — especially in men over 70 or with risk factors.
7. What should I wear to a bone density scan?
Loose, comfortable clothes without metal (like zippers or buttons). You might be asked to change into a gown.
8. Can I eat or drink before the scan?
Yes, there’s no fasting required unless your doctor says otherwise.
9. Do I need a referral for the scan?
Not always. You can often book directly, but check with the clinic or your insurance provider.
10. Where is Delhi Disc & Rheumatology Clinic located?
They’re centrally located in Delhi and easily accessible from surrounding areas. Check their website or Google Maps for directions!