The Benefits of Endoscopic Discectomy for Spinal Relief
Understanding Spinal Problems
Spinal conditions, particularly herniated discs, are a common source of chronic pain and discomfort. When non-invasive treatments such as physical therapy or medication fail, surgical intervention may become necessary. Traditional spinal surgeries often involve large incisions, extended recovery periods and heightened risks of complications. However, advancements in medical technology have paved the way for less invasive techniques with Endoscopic Discectomy emerging as a preferred method for treating spinal issues.
What Is Endoscopic Discectomy?
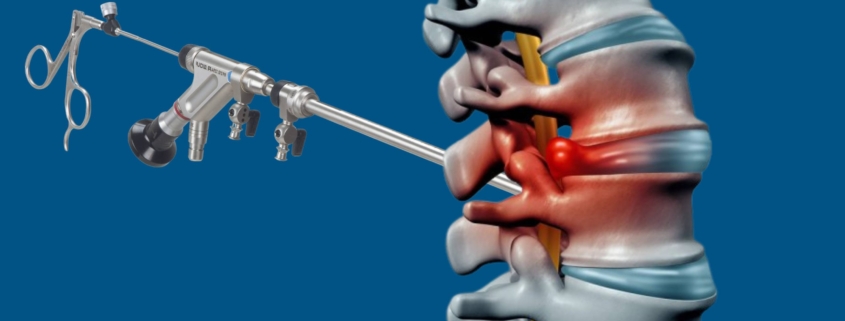
Endoscopic Discectomy is a minimally invasive surgical procedure designed to treat herniated or bulging discs in the spine. It involves the use of an endoscope – a thin, flexible tube with a camera at the end allowing surgeons to access the affected disc through small incisions. Unlike traditional discectomy, which requires large incisions and muscle disruption, this technique offers a more targeted approach to removing the damaged tissue.
By using advanced imaging, the surgeon can precisely locate the herniated disc and remove the portion that is pressing on the spinal cord or nerves, alleviating pain and restoring mobility. The use of an endoscope ensures that the procedure is as minimally invasive as possible, leading to quicker recovery times and fewer complications.
Minimally Invasive Surgery: Key Benefits
The primary advantage of Endoscopic Discectomy lies in its minimally invasive nature. Unlike conventional surgery, which may require extensive cuts, this method involves small incisions often no larger than a few millimeters. This approach significantly reduces the trauma to surrounding tissues, including muscles, ligaments and nerves, contributing to several key benefits.
Reduced Recovery Time
Because of the smaller incisions and less disruption of tissue, recovery time is dramatically shortened. Patients often experience reduced pain, swelling and inflammation, enabling them to return to their normal activities sooner than they would after traditional surgery.
Lower Risk of Complications
Endoscopic Discectomy presents a much lower risk of complications compared to conventional procedures. The small incisions lead to less bleeding and the procedure’s precision minimizes the chance of damaging surrounding structures, such as nerves and blood vessels.
Precision and Accuracy in Treatment
Endoscopic Discectomy stands out for its high level of precision. Surgeons can operate with enhanced visibility thanks to the endoscope, which provides real-time, high-definition images of the spinal region. This enables a more accurate removal of herniated disc material, reducing the chance of leaving residual fragments that could lead to future complications.
Targeted Approach to Herniated Discs
One of the key benefits of this technique is its ability to focus solely on the affected area. Surgeons can carefully and selectively remove the herniated disc material, avoiding damage to the healthy surrounding tissue. This targeted approach leads to better outcomes and faster healing.
Enhanced Surgical Visibility
The endoscope allows the surgeon to view the area in greater detail, providing a clearer view of the spinal structures. This enhanced visibility reduces the risk of surgical errors and increases the overall effectiveness of the procedure.
Faster Recovery: A Game Changer
Perhaps one of the most transformative aspects of Endoscopic Discectomy is its rapid recovery process. Unlike traditional spinal surgeries that may require weeks of bed rest and limited movement, patients undergoing Endoscopic Discectomy can often resume light activities within a few days.
Shorter Hospital Stays
Due to the minimally invasive nature of the procedure, patients typically spend less time in the hospital. In many cases, the surgery is performed on an outpatient basis, meaning patients can go home the same day or the next day.
Return to Normal Activities Sooner
With less postoperative discomfort and faster healing, patients can return to work and their regular activities within weeks, rather than months, as is typical with more invasive spinal surgeries.
Reduced Pain and Postoperative Discomfort
Pain management is a significant concern for patients undergoing spinal surgery. Traditional procedures often involve prolonged postoperative pain due to the larger incisions and muscle disruption. Endoscopic Discectomy, on the other hand, offers a more comfortable recovery experience.
Decreased Nerve Damage Risk
Since Endoscopic Discectomy involves smaller incisions and a more precise surgical approach, there is less risk of nerve damage during the procedure. This reduces the likelihood of postoperative symptoms like numbness or weakness in the limbs.
Improved Pain Management Post-Surgery
Patients often report a significant reduction in pain after Endoscopic Discectomy, as the procedure directly addresses the source of their discomfort without causing excessive trauma to surrounding tissues.
Lower Risk of Infection
Infections are a common concern after any surgery, especially those involving larger incisions. However, the small incisions required for Endoscopic Discectomy significantly reduce the potential for infection.
Smaller Incision, Reduced Exposure
The small size of the incision minimizes the exposed surface area, lowering the risk of infection. Additionally, the procedure is performed in a sterile, controlled environment to further reduce the chance of postoperative infections.
Fewer Chances of Postoperative Complications
Because the surgery is minimally invasive and involves less tissue disruption, the overall risk of complications including infections, blood clots and adverse reactions is lower compared to traditional spinal surgeries.
Cost-Effectiveness of Endoscopic Discectomy
While the upfront costs of Endoscopic Discectomy may be higher due to the specialized equipment and techniques required, the long-term savings can be significant.
Financial Savings for Both Patient and Healthcare Providers
The shorter recovery time means fewer hospital days and a quicker return to work, leading to reduced healthcare costs for the patient. Furthermore, the minimized risk of complications reduces the likelihood of costly follow-up treatments or additional surgeries.
Impact on Long-Term Treatment Costs
Patients who undergo Endoscopic Discectomy may experience fewer long-term issues with their spine, potentially reducing the need for future interventions and chronic pain management.
Patient Satisfaction and Outcomes
Endoscopic Discectomy boasts high success rates, with many patients experiencing significant relief from pain and improved mobility. The procedure’s minimally invasive nature contributes to a more positive patient experience overall.
Success Rates and Positive Feedback
Studies show that the success rates for Endoscopic Discectomy are comparable to, if not better than, traditional spinal surgeries. Patients often report high satisfaction due to the quicker recovery and reduced pain levels post-surgery.
Long-Term Spinal Health Improvements
In many cases, Endoscopic Discectomy can result in long-lasting spinal health improvements, as the procedure addresses the root cause of the pain with minimal disruption to surrounding tissues.
When Is Endoscopic Discectomy the Best Option?
Endoscopic Discectomy is not suitable for every patient. It is most effective for individuals suffering from specific spinal conditions, such as herniated discs or degenerative disc disease, where the disc material is compressing the spinal nerves.
Ideal Candidates for the Procedure
Candidates who are in generally good health, without significant underlying conditions and have a localized herniated disc are ideal for Endoscopic Discectomy.
Limitations and Contraindications
Not everyone is a good candidate for this procedure. For example, patients with multiple herniated discs or severe spinal deformities may require more traditional surgical approaches.
Conclusion: The Future of Spinal Surgery
Endoscopic Discectomy is at the forefront of spinal surgery, offering a minimally invasive alternative that combines precision, speed and effectiveness. As surgical techniques continue to evolve, the future of spinal surgery will likely see even further advancements in minimally invasive approaches, improving outcomes and quality of life for patients.